Abstract
Background: Targeted inhibition of Bruton tyrosine kinase (BTK) has greatly improved the clinical outcomes of patients with chronic lymphocytic leukemia (CLL). Although the only approved BTK inhibitor, ibrutinib, is highly effective in CLL, off-target kinase activity may contribute to adverse effects, which are the most common reason for discontinuation in clinical practice (Mato et al., 2017). Acalabrutinib (ACP-196) is a highly selective, potent, covalent BTK inhibitor in development for hematologic malignancies. A promising safety and efficacy profile was previously reported for acalabrutinib in patients with relapsed/refractory (R/R) CLL/small lymphocytic lymphoma (SLL), including those with high-risk disease, in the ongoing Phase 1/2 ACE-CL-001 study (NCT02029443; Byrd et al., 2016). Here we present an updated analysis of safety and efficacy in this cohort which is now fully enrolled.
Methods: Patients with confirmed CLL/SLL were eligible if they had relapsed after or were refractory to ≥1 prior treatment. Eligible patients were ≥18 years of age with an ECOG performance status (PS) ≤2. Oral acalabrutinib was administered in 28-day cycles at 100-400 mg QD or 100-200 mg BID in the dose-escalation phase of the study and 100 mg BID or 200 mg QD (later switched to 100 mg BID) in the expansion phase. All patients were treated until progressive disease (PD) or unacceptable toxicity. The primary endpoint was safety. Secondary endpoints included investigator-assessed overall response rate (ORR) by International Workshop on Chronic Lymphocytic Leukemia 2008 criteria (Hallek et al., 2008) with modification for lymphocytosis (Cheson et al., 2012), duration of response (DOR) and progression-free survival (PFS). Time to response (TTR) was analyzed as an ad hoc endpoint. Molecular testing for high-risk disease was performed at central clinical laboratories.
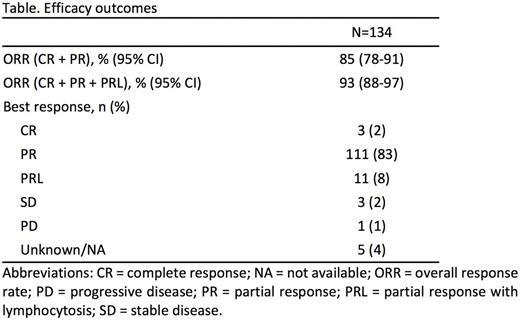
Results: A total of 134 patients (132 with CLL and 2 with SLL) received treatment. The median age was 66 years (range, 42 to 85). Baseline characteristics included ECOG PS ≤1 (97%), bulky lymph nodes ≥5 cm (39%), del(17)(p13.1) in 27/116 (23%) patients, del(11)(q22.3) in 21/116 (18%) patients, unmutated IGHV in 81/111 (73%) patients and β2-microglobulin >3.5 mg/L (75%). The median number of prior therapies was 2 (range, 1-13). The median time on study and follow-up were 19.8 months (range, 0.2-32.4). The ORR (complete response [CR] + partial response [PR]) was 85% and ORR including PR with lymphocytosis (PRL) was 93%; 2% of patients achieved CR (Table). The median TTR was 4.7 months. The median DOR was not reached; the 18-month DOR rate was 85% (95% CI, 72%-92%). The median PFS was also not reached, and the 18-month PFS rate was 88% (95% CI, 81%-93%). ORRs were consistent across high-risk subgroups of del(17)(p13.1) (23/27 [85%]), del(11)(q22.3) (18/21 [86%]) and unmutated IGHV (71/81 [88%]). In patients with del(11)(q22.3) or del(17)(p13.1), the median DOR was not reached, and the 18-month DOR rates were 100% and 71%, respectively. The median PFS was also not reached in patients with del(11)(q22.3) or del(17)(p13.1), and the 18-month PFS rates were 100% and 78%, respectively. The most common adverse events (AEs; ≥20%) of any grade were headache (46%), diarrhea (43%), upper respiratory tract infection (28%), fatigue (27%), nausea (27%), arthralgia and pyrexia (each 23%), contusion (22%) and petechiae and weight increased (each 21%). Grade 3/4 AEs (≥5% of patients) were infrequent and were neutropenia (11%) and pneumonia (10%). Other AEs of interest (any grade/grade ≥3) included hypertension (11%/3%) and atrial fibrillation (3%/2%); no Grade ≥3 bleeding events occurred. Most patients (81%) remain on treatment; the primary reasons for treatment discontinuation were AEs (8%), PD (6%), and death (2%). Richter transformation occurred in 3 patients at 2, 16, and 16 months, respectively. The most common AEs leading to discontinuation were pneumonia (n=3), anemia, neutropenia and thrombocytopenia (n=2 each).
Conclusions: In this updated analysis,treatment with acalabrutinib continues to be associated with high response rates and durable remissions in patients with R/R CLL/SLL, including those with high-risk disease. Reported AEs indicated a tolerable safety profile. Treatment with acalabrutinib is being investigated in patients with R/R CLL in 2 ongoing Phase 3 studies, ACE-CL-006 (NCT02477696) and ACE-CL-309 (NCT02970318).
Byrd: Acerta: Research Funding; Pharmacyclics: Research Funding; Genentech: Research Funding; Janssen: Research Funding. Wierda: Merck: Consultancy, Honoraria; Juno: Research Funding; Genentech/Roche: Consultancy, Honoraria, Research Funding; Janssen: Research Funding; Sanofi: Consultancy, Honoraria; The University of Texas MD Anderson Cancer Center: Employment; Emergent: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Pharmacyclics: Consultancy, Honoraria, Research Funding; Karyopharm: Research Funding; Acerta: Research Funding; Kite: Research Funding; Celgene: Consultancy, Honoraria; Gilead: Consultancy, Honoraria, Research Funding; GSK/Novartis: Consultancy, Honoraria, Research Funding; Genzyme: Consultancy, Honoraria. Schuh: Janssen: Honoraria; Gilead: Honoraria, Research Funding; Roche: Honoraria; Abbvie: Honoraria; Novartis: Honoraria; Celgene: Honoraria; Gilead: Consultancy; Roche: Honoraria; Janssen: Honoraria; Abbvie: Honoraria; Novartis: Honoraria; Celgene: Honoraria. Devereux: MSD: Consultancy, Honoraria; Roche: Consultancy, Other: travel expenses; GSK: Consultancy; Gilead: Consultancy, Honoraria, Other: travel expenses, Speakers Bureau; Janssen: Consultancy, Honoraria, Other: travel expenses, Speakers Bureau; AbbVie: Consultancy, Honoraria; Servier: Other: Advisory board. Chaves: Northwest Medical Specialties, PLLC: Employment. Brown: Pharmacyclics: Consultancy; Roche/Genentech: Consultancy; Astellas Pharma: Consultancy; Infinity Pharmaceuticals: Consultancy; Celgene: Consultancy; Pfizer: Consultancy; Sun BioPharma: Consultancy, Research Funding; Janssen: Consultancy; AstraZeneca: Consultancy; Janssen Oncology: Honoraria; AbbVie: Consultancy, Honoraria; Redx: Consultancy; Gilead: Consultancy, Research Funding. Hillmen: Pharmacyclics LLC, an AbbVie Company: Honoraria, Research Funding; Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Research Funding; GSK: Consultancy, Honoraria, Research Funding; Roche: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Gilead: Consultancy, Honoraria, Research Funding; Celgene: Research Funding; Novartis: Honoraria, Research Funding. Martin: Janssen/Pharmacyclics: Consultancy; Genentech: Consultancy; Bayer: Consultancy; Gilead: Consultancy; Verastem: Consultancy; Novartis: Consultancy; Celgene: Research Funding; Teva: Research Funding. Ghia: Roche: Consultancy, Honoraria; Pharmacyclics: Consultancy, Honoraria; Novartis: Research Funding; Janssen: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Gilead: Consultancy, Honoraria, Research Funding, Speakers Bureau; Adaptive: Consultancy. Barrientos: Abbvie/Pharmacyclics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Gilead: Membership on an entity's Board of Directors or advisory committees, Research Funding; Acerta Pharma: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees. Pagel: Gilead: Consultancy; Pharmacyclics: Consultancy. Woyach: Janssen: Honoraria; Karyopharm Inc: Research Funding; Morphosys Inc: Research Funding. Charuworn: Acerta Pharma: Employment. Hamdy: Acerta Pharma: Employment, Equity Ownership, Patents & Royalties: Acalabrutinib related patents. Izumi: Acerta Pharma: Employment, Equity Ownership. Patel: Acerta Pharma: Employment. Rothbaum: Acerta Pharma: Employment, Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; Quogue BioVentures II LLC: Equity Ownership. Wang: Astra Zeneca: Equity Ownership; Acerta Pharma: Employment, Equity Ownership. Furman: Pharmacyclics: Consultancy; Abbvie: Consultancy; Genentech: Consultancy; Gilead: Consultancy; Sunesis: Consultancy; Verastim: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal